Disclaimer: Our stories have been researched and fact-checked to the best of our abilities. Should you spot
mistakes, inaccuracies, or have queries about our sources, please drop us an e-mail at
hello@kontinentalist.com
Credits
Code / Siti Aishah
Data / Doctors without Borders
Design / Amanda Teo
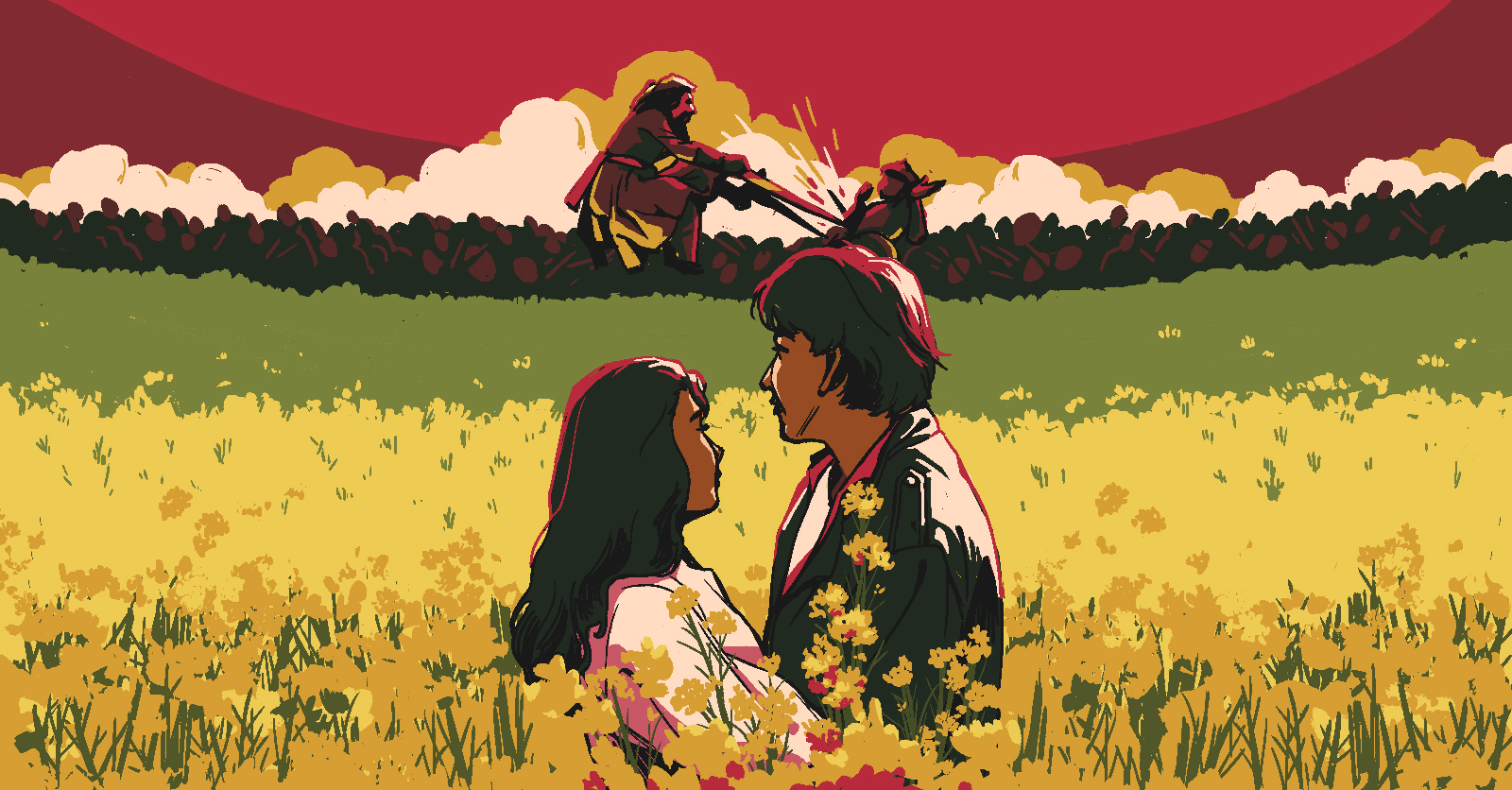
Illustration / Griselda Gabriele
Story / Zafirah Zein
Recommended Stories